03 June 2025
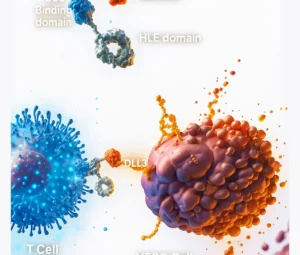
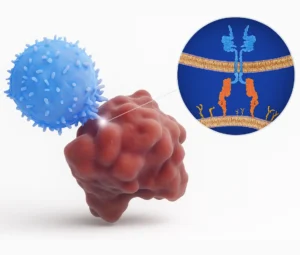
Large B-cell lymphoma (LBCL) is an aggressive malignancy of mature B cells. Autologous CAR-T therapy—where a patient’s own T cells are engineered to express a chimeric antigen receptor (CAR) targeting CD19—has revolutionized treatment, but its manufacture requires weeks and is compromised when patients’ T cells are weakened by prior treatments. Allogeneic, “off-the-shelf” CAR-T cells offer a ready alternative derived from healthy donors, potentially enabling immediate treatment and consistent product quality.
Cemacabtagene ansegedleucel (cema-cel, also known as ALLO-501) exemplifies this approach. Donor T cells are edited at the T-cell receptor alpha constant (TRAC) locus to prevent graft-versus-host disease (GVHD) and at the CD52 gene to resist the lymphodepleting antibody ALLO-647. This “double knockout” design both curtails GVHD and allows selective host conditioning, creating space for the incoming CAR-T cells.
The combined Phase I ALPHA and ALPHA2 trials enrolled 33 patients with relapsed/refractory LBCL who had not received prior CAR-T therapy. After a lymphodepletion regimen of fludarabine, cyclophosphamide, and ALLO-647, participants received a single infusion of cema-cel. Patient characteristics included a median of three prior therapies and rapidly progressive disease. The overall response rate (ORR) was 58%, with a 42% complete response (CR) rate. Among responders, median duration of response reached 23.1 months, and CAR-T cells persisted for up to four months post-infusion.
Safety outcomes were notable for the absence of GVHD and no Grade ≥3 cytokine release syndrome (CRS) or neurotoxicity (ICANS). The most frequent adverse events were predictable hematologic toxicities—neutropenia and anemia—related to the conditioning regimen. No unexpected toxicities emerged.
Key advantages include rapid treatment initiation—a median two-day window from enrollment to infusion—contrasting sharply with autologous manufacturing delays. A standardized allogeneic product also delivers consistent potency and may broaden access, especially at centers lacking cell-processing facilities or for patients whose T cells are suboptimal. Scalability data indicate a single manufacturing run could produce roughly 100 doses, paving the way for greater treatment availability and potential cost reductions.
Moving forward, larger randomized Phase II/III trials will compare cema-cel to autologous CAR-T and standard therapies in LBCL, validating efficacy, durability, and long-term safety. Future studies may explore optimized dosing, consolidation strategies (e.g., second infusions), and integration into earlier lines of therapy.
Allogeneic CAR-T therapies like cema-cel mark a significant advance in immuno-oncology, addressing logistical and biological hurdles of personalized CAR-T while offering rapid, uniform, and potentially more accessible treatments for patients with aggressive lymphomas.
References:
- Locke FL, Munoz JL, Tees MT, Lekakis LJ, de Vos S, Nath R, Stevens DA, Malik SA, Shouse GP, Hamadani M, Oluwole OO. Allogeneic Chimeric Antigen Receptor T-Cell Products Cemacabtagene Ansegedleucel/ALLO-501 in Relapsed/Refractory Large B-Cell Lymphoma: Phase I Experience From the ALPHA2/ALPHA Clinical Studies. Journal of Clinical Oncology. 2025 Feb 13;43(14):1695.
- ALPHA-2 Study Protocol: A SINGLE-ARM, OPEN-LABEL, PHASE 1/2 STUDY EVALUATING THE SAFETY, EFFICACY, AND CELLULAR KINETICS/PHARMACODYNAMICS OF ALLO501A, AN ANTI-CD19 ALLOGENEIC CAR T CELL THERAPY, AND ALLO-647, AN ANTI-CD52 MONOCLONAL ANTIBODY, IN SUBJECTS WITH RELAPSED/REFRACTORY LARGE B-CELL LYMPHOMA (LBCL). NCT04416984.