03 June 2025
Immune thrombocytopenia (ITP) is an autoimmune disorder marked by platelet destruction, leading to bleeding and bruising. Standard therapies (steroids, rituximab, thrombopoietin receptor agonists) fail in a subset of patients, leaving persistent severe thrombocytopenia. CAR-T cell therapy targeting CD19—a marker present from B-cell progenitors through plasmablasts—promises deeper, more comprehensive depletion of autoantibody-producing cells than CD20-directed treatments.
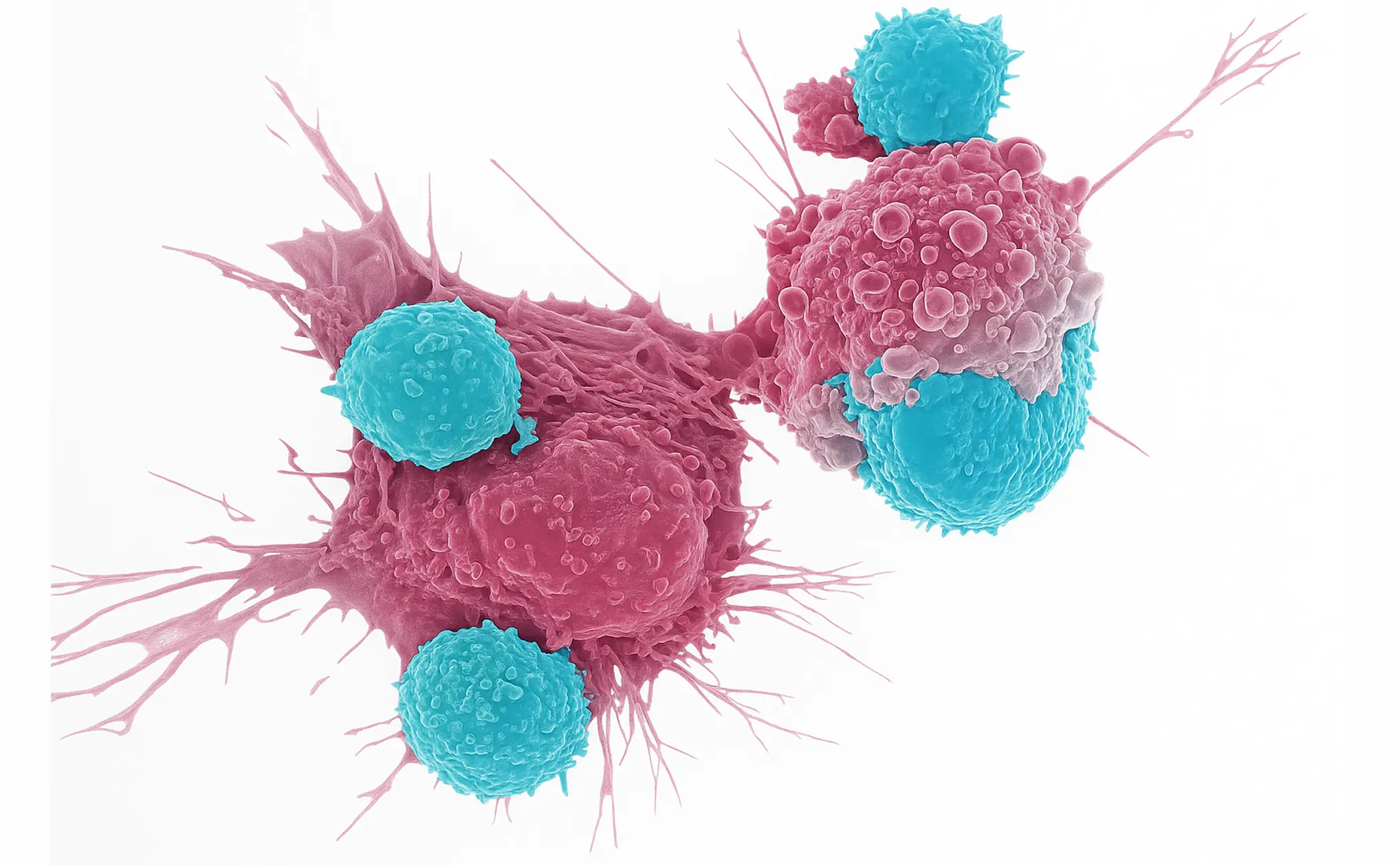
Preclinical murine models of ITP offered proof of concept: CD19 CAR-T infusion accelerated platelet recovery, depleted CD19+ B cells and CD138+ plasma cells in the spleen, and reduced anti-platelet autoantibodies. Regulatory T-cell populations increased, suggesting broader immunomodulation. Safety appeared favorable, with no severe cytokine release syndrome (CRS) noted. In vitro co-cultures of human spleen cells from ITP patients further confirmed effective removal of B-cell subsets.
Early clinical case reports underscore potential. A 38-year-old woman with refractory ITP in systemic lupus erythematosus had failed high-dose steroids, immunosuppressants, rituximab, and thrombopoietin agonists over nearly a decade. She received autologous CD19 CAR-T cells (inati-cel) following standard lymphodepletion. B cells were eradicated, and platelet counts rose into a safe range within two months, remaining stable at six months. Only a transient, mild (Grade 1) fever occurred, resolving without intervention.
In a second case, a 35-year-old man with multi-refractory primary ITP post-splenectomy received autologous CD19 CAR-T (KYV-101). His platelet count normalized by day 42, allowing discontinuation of all ITP medications, and remained at normal levels at four months. Pathogenic autoantibodies disappeared, and chronic fatigue resolved. He experienced Grade 1 CRS managed with a single tocilizumab dose. As B cells reemerged, they were mainly naive, suggesting a durable “reset” of the B-cell compartment.
These reports indicate that profound, sustained B-cell depletion by CD19 CAR-T cells can halt autoantibody production and restore platelet counts in refractory ITP. Side effects—primarily mild CRS—appear more manageable than in malignancy settings, likely owing to lower antigen burden. Neurotoxicity has not been reported in these small cohorts.
Critical questions remain: optimal CAR construct and dosing, patient selection criteria, long-term B-cell reconstitution dynamics, infection risk following deep immunosuppression, and durability of remission. Larger, controlled clinical trials are essential to evaluate safety, efficacy, and cost-effectiveness, and to define the role of CAR-T in the ITP treatment algorithm.
Nevertheless, these early successes herald a new paradigm in autoimmune therapy: reprogramming the immune system by targeting disease-causing B cells at their source. If validated in larger studies, CD19 CAR-T could become a transformative option for patients with the most refractory forms of ITP.
References:
- Trautmann-Grill K, von Bonin M, Georgi A, Middeke JM, Böttcher M, Meyer O, Borie D, Bornhäuser M, Mikusko M, Wolleschak D, Mougiakakos D. Salvage treatment of multi-refractory primary immune thrombocytopenia with CD19 CAR T cells. The Lancet. 2025 Jan 4;405(10472):25-8.
- Wang Y, Han F, Guo Q, Feng Q, Peng J, Hou M, Xu M. The Therapeutic Efficacy of CD19 Chimeric Antigen Receptor T Cells in Immune Thrombocytopenia Model. Blood. 2023 Nov 2;142:688.
- Han F, Jiang Z, Guo Q, Li Y, Li C, Liang X, Han L, Gallant RC, Hou M, Peng J, Xu M. CD19 chimeric antigen receptor‐T cell therapy in murine immune thrombocytopenia. British Journal of Haematology. 2025 May;206(5):1430-42.
- Li M, Zhang Y, Jiang N, Ning C, Wang Q, Xu D, Wang Z, Lv L, Zhou D, Zeng X. Anti–CD19 CAR T cells in refractory immune thrombocytopenia of SLE. New England Journal of Medicine. 2024 Jul 25;391(4):376-8.