15th December, 2024
The other day, while I was sitting in my OPD, a worried couple came to see me. The wife was anxious that she might develop cancer since many of her family members had experienced it. She wanted to know if she or her children might be prone to cancer, whether it could be detected early, and if effective treatment options were available.
This brings us to an important topic: Hereditary Cancers.
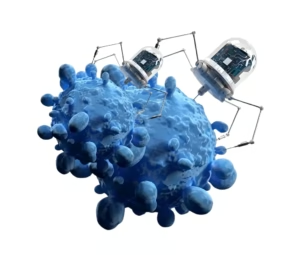
Cancer is essentially a disease of tissue growth regulation. It involves uncontrolled cell growth in any tissue of the body, leading to local tissue damage, secretion of toxic substances, and sometimes spreading to other organs. This uncontrolled growth reduces the functionality of normal tissues. Some cancers grow rapidly, while others progress more slowly.

Most Cancers Are Not Inherited
Most cancers are not inherited. They are caused by genetic alterations acquired during a person’s lifetime. Factors such as tobacco use, alcohol consumption, radiation exposure, chemical exposure, lifestyle, diet, and obesity contribute significantly to cancer risk. These cancers occur by chance, much like an accident.
What Does It Mean When Cancer Is Hereditary?
Hereditary cancer occurs when one or more genes increase an individual’s predisposition to developing cancer. However, hereditary cancers account for only about 5-10% of all cancer cases. Individuals with hereditary cancer may develop cancer earlier or later in life and have an increased lifetime risk of developing cancer in one or more organs.
Indicators of Hereditary Cancer:
1. Early-Onset Cancer: Cancer occurring at a younger-than-usual age for that type.
2. Multiple Affected Family Members: Several family members diagnosed with cancer.
3. Bilateral Cancers: Cancer affecting both paired organs (e.g., both breasts).
4. Multiple Cancer Types in One Individual: A family member with more than one type of cancer.
Types of Cancers Most Likely to Be Hereditary:
- Breast cancer
- Colorectal cancer
- Stomach cancer
- Prostate cancer
- Neuroendocrine
- cancers (e.g., thyroid, adrenal glands)
Diagnosis: Genetic Counseling and Testing
If hereditary cancer is suspected, the treating doctor will review detailed personal and family histories before recommending genetic counseling and testing. These tests, performed using blood or buccal swab samples, are non-invasive but can be expensive.
A positive test result does not mean that the individual has cancer; rather, it indicates an increased risk. Regular follow-up is crucial. Genetic counseling before testing helps individuals understand the benefits, limitations, and potential social and personal implications of the results. Random testing without proper guidance is not advisable.
Preventive and Treatment Options for Hereditary Cancer:
For individuals prone to hereditary cancer, preventive and treatment measures include:
- Regular Screenings: Colonoscopy, breast screenings, and biopsies of suspicious lesions.
- Medication: Taking aspirin under medical supervision.
- Prophylactic Surgery: Removing at-risk organs to prevent cancer development.
Understanding hereditary cancer is key to early detection and prevention. If you suspect a family history of cancer, consult a healthcare professional for guidance on genetic counseling and testing. Early intervention can make a significant difference in outcomes.