12 December 2025
Blood is often called the ‘river of life’, and for good reason. It connects every organ in the human body, delivering oxygen, fighting infection, and repairing damage. When this complex system functions correctly, it goes unnoticed. However, when the balance is disturbed, it can lead to a variety of medical conditions. This blog series aims to simplify the science behind these conditions, offering a clear understanding of how blood diseases develop and how modern medicine addresses them.
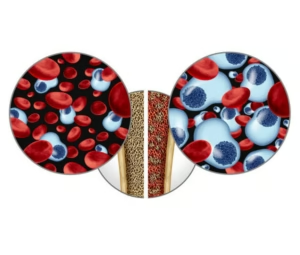
To understand blood disorders, one must first look at where blood is made. Deep inside the bones lies a spongy tissue known as bone marrow. This can be described as the body’s manufacturing plant. It contains ‘mother cells’, scientifically known as stem cells, which have the unique ability to divide and mature into different types of blood cells. In a healthy individual, this process is perfectly regulated, constantly releasing three main components into the bloodstream. Red blood cells act as transport vehicles, carrying oxygen to tissues; white blood cells serve as the body’s defence force against bacteria and viruses; and platelets function as a repair crew, clustering together to stop bleeding when an injury occurs.
Hematological diseases — disorders of the blood — usually arise when this manufacturing process in the bone marrow encounters an error. These errors can generally be divided into two categories. The first category involves conditions where the body simply does not have enough healthy cells. For example, in cases of anaemia, there is a shortage of red blood cells, leading to fatigue. Similarly, in conditions like Immune Thrombocytopenia (ITP), the body’s own immune system mistakenly identifies platelets as foreign invaders and destroys them, leaving too few behind to stop bleeding effectively.
The second category involves conditions where the bone marrow produces abnormal cells that grow out of control. These are often referred to as haematological malignancies or blood cancers. Leukaemia, for instance, occurs when the marrow produces excessive, abnormal white blood cells that crowd out the healthy ones. Lymphoma affects the lymphatic system, a specific part of the immune defence, while Multiple Myeloma impacts plasma cells. While these names can sound intimidating, understanding the mechanism—that it is essentially a ‘production line’ error — is the first step in making sense of the diagnosis.
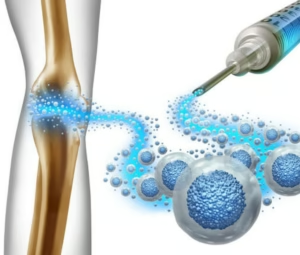
Fortunately, the field of Hematology is rapidly advancing. Treatments have evolved significantly from the early days of standard chemotherapy. Medical science now utilises Cellular Therapy, which includes procedures like bone marrow and stem cell transplants. There are also newer approaches such as Immunotherapy and Targeted Therapy, which focus on training the body’s own immune system to recognise and remove abnormal cells.
Over the coming months, this blog will serve as a resource to explore these topics in greater depth. Future articles will look closely at specific conditions, such as Acute Myeloid Leukaemia and various types of Lymphoma, as well as explaining the details of treatments like stem cell transplantation. The goal is to provide accessible information that demystifies these complex diseases, helping readers navigate the world of haematological health with greater confidence and clarity