3 January 2026
Hearing “blood problem” about your child can feel overwhelming. But blood disorders in children aren’t one single disease. They’re a spectrum—from very common issues like iron deficiency anemia to less common conditions that need specialist care.
What is blood made of?
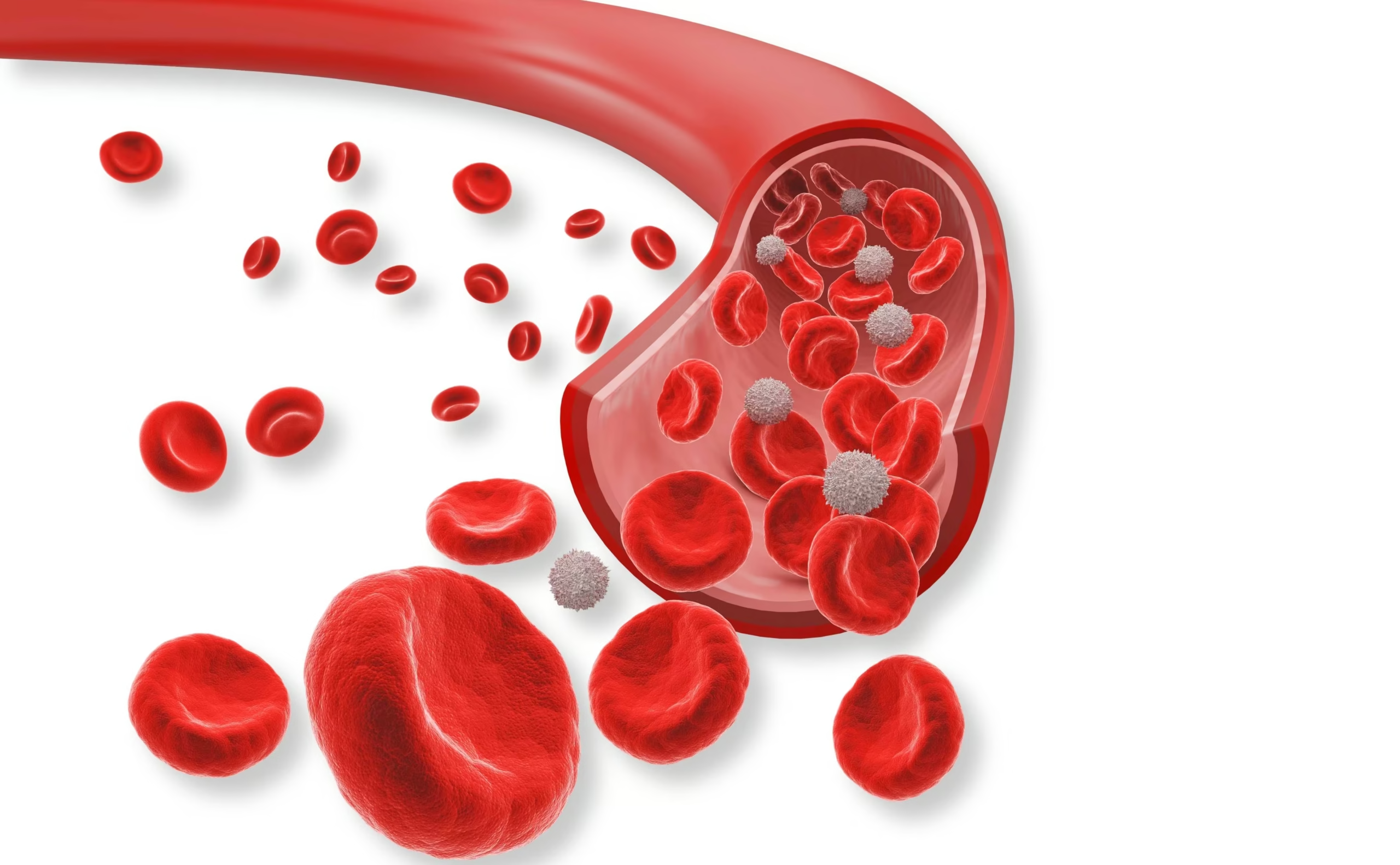
Blood has three main “teams”:
- Red blood cells: carry and supply oxygen to all organs
- White blood cells: fight infections
- Platelets: helps stop bleeding and easy bruising
A blood disorder happens when one of these is too low, too high or not working properly.
Red blood cell problems or “Anemia”
What parents may notice
- Child looks pale (palms, lips)
- Tired, less playful, sleepy
- Poor appetite
- Breathless or tired quickly while playing
- Sore mouth/bright red tongue
- Developmental delay (infants)
Causes
- Iron deficiency (very common, especially during growth spurts)
- B12/folate deficiency – Vegetarians, goat milk consumption
- After infections (autoimmune anemia)
- Inherited conditions like thalassemia or sickle cell disease
- Aplastic anemia
- Chronic kidney disease
- During chemotherapy/radiation therapy
Platelet problems or “Thrombocytopenia”
What parents may notice
- Unexplained bruises, tiny pin-point red spots on skin
- Frequent nosebleeds
- Gum bleeding while brushing
- Heavy periods in teens
- Bleeding that lasts “too long” after a cut or tooth extraction
Causes
- ITP (Immune Thrombocytopenia): often happens after a viral illness, vaccination. Usually resolves in few weeks to months. May persist in a few cases.
- Low platelets during/after infections : Infections like dengue, malaria can reduce body’s platelet counts. Some viruses can temporarily affect bone marrow and cause reduce platelets.
- Inherited conditions : Certain genetic conditions which lead to a defective bone marrow and hampered platelet production.
- Bleeding/clotting factor issues (like hemophilia or von Willebrand disease): platelets
- may be normal but clotting factors (factor VIII,IX etc) may be deficient.
- During chemotherapy/radiation therapy
White blood cell problems : Leucopenia
What parents may notice
- Unusually frequent or severe infection requiring hospitalisation
- Recurrent pneumonias
- Severe infections starting from early infancy
- Persistent fevers
- Repeated mouth ulcers
- Poor growth
- Chronic diarrhoea
The “master” problem : Defective bone marrow
Bone marrow is contained in the hollow space inside our bones
It consists of “stem cells” which makes all three types of blood cells – RBC, WBC and platelets.
Some inherited and acquired conditions can affect the bone marrow and reduce the production of blood cells, leading to low blood counts.
In illnesses such as leukemia, the marrow can become crowded with too many abnormal, immature white blood cells, which don’t work properly and leave less space for healthy blood cell production.
Diagnosis & Treatment
What tests do doctors usually do first?
Most children need simple blood tests :
- CBC (Complete Blood Count): checks hemoglobin, white cells, platelets
- Peripheral smear: microscope look at cells count and shape
- Iron studies (if peripheral smear is inconclusive)
- Reticulocyte count (how actively the body is making new red cells)
- Hemoglobin electrophoresis – to look for abnormally formed hemoglobin as in thalassemia or sickle cell anemia
- PT/INR and aPTT – to screen for coagulation problems
The doctor may ask for further tests based on these reports and the suspected diagnosis.
Few myths on blood disorders
- Low hemoglobin always requires blood transfusions
Even when hemoglobin is very low, many nutritional anemias do not require a blood transfusion if the child is otherwise clinically stable. Oral supplements and dietary correction are often sufficient. It’s best to seek an opinion from a pediatric hematologist to guide the safest plan.
- All children with low hemoglobin should be given iron supplements
Low hemoglobin can occur due to many different reasons. In conditions like thalassemia, the body may already have excess iron, so giving iron supplements unnecessarily can be harmful. That’s why a careful evaluation and a clear management plan from a pediatric hematologist are essential when treating low hemoglobin.
- Bleeding from nose is due cold or cold weather
Cold weather increases scaling but recurrent nose bleeding should be evaluated
- Papaya leaf extract can increase platelet counts
Low platelet counts can happen due to a variety of reasons and treatment depends on the cause
- A good diet can fix everything
A balanced diet can certainly improve overall health and wellbeing, but it may not be enough to fully correct a blood disorder. In nutritional anemia, additional supplements are often needed along with dietary changes to restore levels effectively.
Blood disorders in children can range from mild and temporary to more serious conditions, and treatment always depends on the underlying cause and the severity of symptoms and not just the blood count on a report.