3 January 2026
Blood cancer affecting the white blood cells — leukemia— remains one of the most challenging diagnoses a patient can receive. Yet modern medicine has transformed this once uniformly fatal disease into one where cure is increasingly possible. At the heart of this transformation lies bone marrow transplantation, a procedure that offers hope to thousands of Indian patients each year.
Leukemia develops when the bone marrow begins producing abnormal white blood cells that multiply uncontrollably. These abnormal cells crowd out healthy blood cells, leaving patients vulnerable to infections, anaemia, and bleeding problems. Some leukemias progress rapidly within weeks, whilst others develop slowly over months or years.
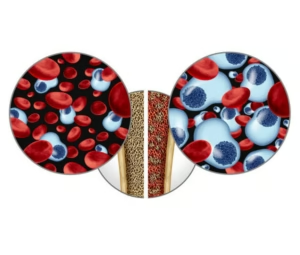
When chemotherapy alone cannot control the disease, or when leukemia returns after initial treatment, doctors may recommend a bone marrow transplant—also called a stem cell transplant. This procedure essentially replaces the patient’s diseased bone marrow with healthy stem cells that can grow into normal blood cells.
There are two main types of transplants. In an autologous transplant, doctors collect the patient’s own stem cells during remission, store them, and return them after high-dose chemotherapy. This approach works well for certain types of leukemia where the patient’s own cells can be safely harvested. In an allogeneic transplant, stem cells come from a donor—often a sibling, family member, or matched unrelated donor from a registry.
The transplant journey begins weeks before the actual procedure. Patients undergo conditioning therapy, which uses high-dose chemotherapy or radiation to destroy the diseased bone marrow and make space for new cells. This phase is physically demanding, and patients often stay in hospital under close monitoring.
The transplant itself is surprisingly straightforward—stem cells are infused through a central line, much like a blood transfusion. These cells find their way to the bone marrow, where they begin the remarkable process of engraftment, essentially setting up a new blood cell factory. This typically takes two to four weeks, during which patients remain highly vulnerable to infections.
Recovery extends well beyond the hospital stay. The first 100 days are critical, with patients requiring frequent monitoring for complications like graft-versus-host disease (in allogeneic transplants), infections, and organ problems. Full immune system recovery can take six months to a year, sometimes longer.
Success rates have improved dramatically. For acute leukemias transplanted during first remission, cure rates can exceed 50-70%, depending on various factors like age, disease type, and donor match quality. Even patients with relapsed disease often achieve long-term remission.
The procedure demands much from patients and families—financial resources, emotional resilience, and strong support systems. However, India’s growing network of transplant centres, improving insurance coverage, and government schemes have made this life-saving treatment increasingly accessible.
For many patients, a bone marrow transplant represents not just treatment, but a complete reset—a chance to restart life with a healthy blood system. Whilst the journey is arduous, the destination offers something precious: the possibility of cure and a return to normal life.