17 January 2026
Hereditary blood disorders are conditions passed from parents to children through genes and affect the production or function of blood cells. Diseases such as sickle cell disease, thalassemia, hemophilia, and certain inherited immune deficiencies can cause lifelong health problems, repeated hospitalizations, and a significant impact on quality of life. For decades, treatment focused mainly on managing symptoms rather than addressing the root cause but the faulty gene itself.
Today, gene therapy is changing that narrative by offering the possibility of long-term or even curative treatment.
Understanding Hereditary Blood Disorders
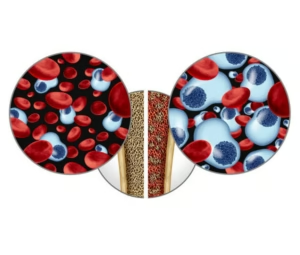
These disorders arise from mutations in genes responsible for making hemoglobin, clotting factors, or immune cells. For example, sickle cell disease and beta-thalassemia result from defects in the hemoglobin gene, leading to anaemia and organ damage, while hemophilia is caused by missing or defective clotting factors that result in uncontrolled bleeding. Because these conditions originate in the bone marrow, they are particularly well suited for gene-based approaches.
What Is Gene Therapy?
Gene therapy works by repairing or compensating for the faulty gene. In many cases, doctors collect a patient’s own blood-forming stem cells, correct the genetic problem in the laboratory, and then return these modified cells to the patient. Once inside the body, the corrected cells can start producing healthy blood cells for years. Whereas, some gene therapies add a working copy of the missing gene, while others use precise gene-editing tools to switch genes on or off. For example, certain therapies help the body make fetal hemoglobin, a natural form of hemoglobin present before birth that can replace the defective adult version.
Gene Therapy in Action
Gene therapy is no longer experimental. Several treatments have now been approved by regulatory authorities, marking a turning point in medicine. Gene therapy has already shown transformative results in conditions like sickle cell disease and beta-thalassemia, where treated patients have experienced dramatic reductions in disease symptoms and, in some cases, freedom from regular transfusions. In hemophilia, gene therapy has enabled sustained production of clotting factors, significantly reducing bleeding episodes and the need for lifelong injections. These successes demonstrate that treating the genetic root of disease is not just theoretical it is becoming a clinical reality.
Challenges and Considerations
Despite its promise, gene therapy is not without challenges. The treatment process is complex, expensive, and requires specialized medical centres. There are also long-term safety considerations, including durability of gene expression and potential immune reactions. Ensuring global access, especially in regions where hereditary blood disorders are most prevalent, remains a major hurdle.
The Road Ahead
The future of gene therapy for hereditary blood disorders lies in safer, more precise, and more accessible technologies. Researchers are working to reduce treatment intensity, improve manufacturing efficiency, and explore in vivo gene therapies that may one day eliminate the need for stem cell transplantation altogether.
In conclusion, hereditary blood disorders were once considered lifelong conditions with limited treatment options now Gene therapy is redefining that outlook by addressing disease at its genetic source. While challenges remain, the field is rapidly advancing toward a future where durable, potentially curative treatments become widely available offering renewed hope to patients and families worldwide.